OPINIONS
Anna Kynthia Bousdoukou
Finding a way out of the labyrinth from mental illness to mental health

March 16 2022
Approximately one in four people experience mental illness each year, with close to 1 billion people living with a diagnosable mental disorder. Apart from the substantial financial burden, mental illness is one of the leading causes of disability, as well as premature death (as much as two decades early) due to preventable physical ailments, while suicide is the second leading cause of death among young people. People with mental illness also experience widespread human rights abuse, discrimination and stigma.
Health systems all over the world have not yet effectively responded to the financial, medical and societal burden of mental disorders. Between 76% and 85% of people with severe mental disorders receive no treatment for their disorder in low and middle-income countries and between 35% and 50% in high-income countries. Part of this gap in care is due to the scarcity of resources within countries to meet mental health needs, as well as the inequitable distribution and inefficient use of such resources, which hinders access to care. In addition, many patients reject care because of the insidious nature of mental illness that often impedes its own treatment (many people with schizophrenia do not realize they have an illness), as well as because they fear the repercussions and stigma. Further compounding problems are the poor quality of care, the ineffectiveness of many available treatments and the lack of long-term engagement for those receiving them. Only a fraction of those with access to care receive minimally adequate (by current scientific standards) treatments that correspond to the patient's level of need. Many people receiving medication do not take it and, among those who take it, only a small fraction responds to it. The end result is that only 5-10% of those with access to care get well.
The Covid-19 pandemic and the unprecedented mental health crisis it caused served as a “stress-test” that revealed how broken and vulnerable mental health care systems are world-wide. A massive investment in mental health is urgently needed on three fronts: First, there is a need for targeted efforts to increase mental health awareness and reduce the stigma, which is fueled by misunderstandings of mental illness etiology and stereotypic beliefs. Incorporating mental health education into a comprehensive health education curriculum at schools has the potential to destigmatize mental illness, augment the awareness and skills needed for prevention and encourage help-seeking. Second, there is a need to expand and expedite deployment of available treatments and interventions, as well as of social support and long-term recovery care mechanisms. While technology cannot and should not substitute the need of human interaction, virtual connections of mental health professionals through implementation of telepsychiatry may facilitate wider deployment of care especially in rural and underserved populations. Third, there is an urgent need for research to improve existing treatments and, most importantly, identify new treatments for mental disorders by linking together new scientific discoveries, bold vision and scientific rigor.
The modern resurrection of efforts to develop therapies for psychiatric disorders has the potential to shape the future of psychiatric care in a profound way, but must respect the lessons learned from the mid-twentieth century, regarding not only the clinical, but also the social ramifications of poor scientific rigor. As a doctor and neuroscientist who has studied schizophrenia for decades, I find the story of chlorpromazine (also known by its trade name, Thorazine) quite didactic: originally an antihistamine, it was first repurposed as an antianxiety medication and found to reduce agitation, hallucinations and delusions in psychotic patients. By mid-1950s, it was reborn as an antipsychotic, being compared to the use of penicillin for infectious diseases and promoting for the first time the notion that mental illness could be cured with medication. Enthusiasm for Thorazine, which entered clinical practice without any supporting clinical trials, significantly accelerated the process of deinstitutionalization that started soon after the end of World War II and culminated in the 1960s and signified a diversion of mental health care away from asylums into community mental-health centers. The fact that Thorazine did not live up to its promise as a miracle cure, along with the fact that many countries closed mental institutions without carefully coordinating the creation of community mental-health centers, severely limited access to care, creating a new crisis that reverberates until today in the form of homelessness, marginalization, incarceration and crowding of emergency rooms.
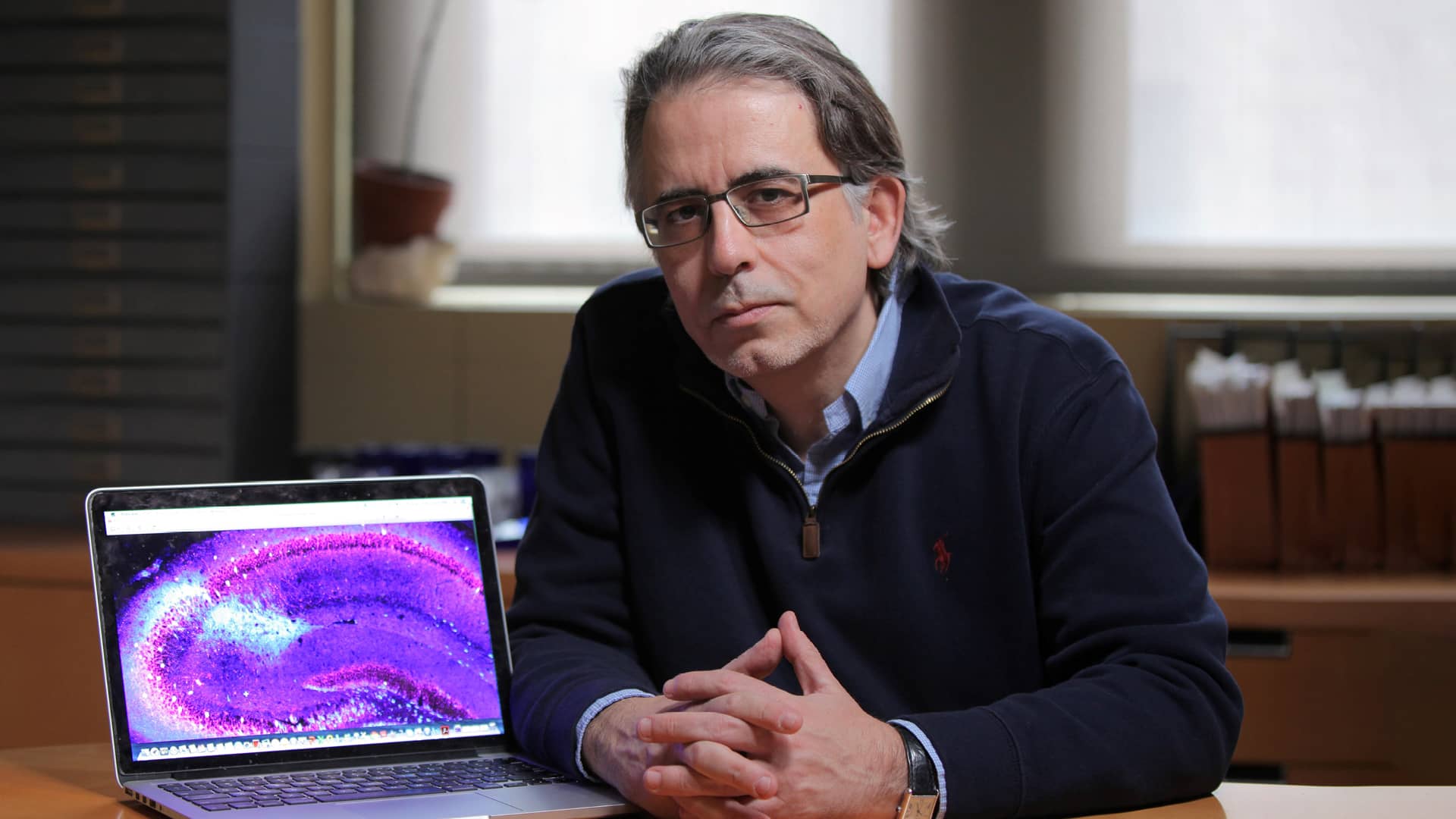
Discovery of chlorpromazine happened largely by chance in an era when knowledge of the mechanisms underlying mental illnesses were too rudimentary. Dramatic progress achieved during the past 10-15 years in integrating genomics and neuroscience into psychiatry has enhanced our understanding of the genetic architecture of psychiatric disorders (what kind and how many different mutations increase the risk for psychiatric disorders) and provided fresh insights into their pathophysiology (what kind of failures in brain circuits lead to its symptoms). The complex biological nature of psychiatric disorders still poses challenges but this newly acquired knowledge has provided a platform to develop and test in a rigorous manner novel treatments and interventions that can be targeted with a degree of specificity and fewer side effects to individual patients or groups of patients who share genetic liabilities or other pathophysiological markers. Seventy years after chlorpromazine became first available (in November 1952), the good news is that, learning from our successes and failures, as well as from the collective wisdom of almost all other medical disciplines, we now have a realistic opportunity, a roadmap and a commitment to implement a genuine transformation on psychiatric disease treatment.

